Paving the Way to Healthcare Equity: A Comprehensive Review of Care Gaps and Emerging Initiatives in Dermatology
A snapshot of the current dermatological care landscape for patients with with Skin of color (SOC) and proposes a structured framework for evaluating outcomes and guiding future initiatives addressing historically overlooked considerations.

Andrew Alexis, Raj Chovatiya, Susan Taylor, Nada Elbuluk, Chesahna Kindred, Amber R. Atwater, Meena Hansen, Maria Jose Rueda, Tanja Bosshard Becker, Vivian Shi & Seemal R. Desai
This work highlights the persistent and deeply rooted disparities affecting dermatological care for patients with skin of color (SOC) in the United States, despite increasing awareness of inequities across the healthcare system. By examining the cultural, socioeconomic, and structural factors—including racial and ethnic biases and the long-standing underrepresentation of SOC in research and medical training—that contribute to these care gaps, this article underscores the urgent need for sustained, multifaceted solutions. Although medical societies, pharmaceutical companies, and patient organizations have introduced a wide range of initiatives aimed at improving equity, several challenges remain in enhancing clinician communication, strengthening cultural competence, refining skin type classification systems, and ensuring the accuracy of artificial intelligence–driven diagnostic tools for SOC populations. The significance of this work lies in its call for rigorous, future-focused research to evaluate the long-term effectiveness of these initiatives in reducing disparities, improving outcomes, and advancing equitable dermatological care for patients with SOC.
Abstract
Historically, dermatology research and clinical practice in the United States (USA) have overlooked important considerations in the dermatological care of individuals with skin of color (SOC). With growing awareness of the disparities in health outcomes among racial and ethnic groups, it is critical to recognize the existing care gaps and implement initiatives that promote healthcare equity. To identify the unmet dermatological needs of these populations, a literature review was conducted from January 2020 to October 2023, which revealed 18 distinct dermatological care gaps categorized under four root causes: cultural diversity, income status, racial bias, and underrepresentation in medical and research settings. An initiative scan was performed using a similar search and prioritization strategy to assess ongoing activities led by medical societies, pharmaceutical companies, and patient organizations to address these care gaps. Sustaining these evidence-based interventions is essential to reducing racial and ethnic disparities in dermatology and driving meaningful change in the healthcare system within the USA. This review offers a snapshot of the current dermatological care landscape for patients with SOC and proposes a structured framework for evaluating outcomes and guiding future initiatives.
Key Summary Points
- Despite growing awareness of healthcare disparities among racial and ethnic minorities in the United States, significant gaps persist in the dermatological care of patients with skin of color (SOC).
- Within the field of dermatology, the most prominent care gaps for patients with SOC are caused by cultural diversity, socioeconomic disadvantage, racial and ethnic biases, and underrepresentation in medical research and training.
- In response to existing care gaps in dermatology, a range of initiatives—including conferences, mentorship programs, and scholarships—have been launched by medical societies, pharmaceutical companies, and patient organizations.
- While hundreds of initiatives have been implemented to address disparities in dermatological care, fundamental challenges remain, particularly in enhancing healthcare professional communication, fostering cultural competence, refining skin type classification scales, and improving accuracy of artificial intelligence-driven diagnostic tools for patients with SOC.
- Future research should evaluate the long-term effectiveness of initiatives in reducing disparities, improving patient outcomes, and fostering more equitable access to dermatological care among patients with SOC to accurately assess their real-world impact.
Introduction
By 2042, more than half of all Americans are predicted to belong to a minority group characterized by skin of color (SOC) [1, 2]. While a precise definition of SOC remains to be widely adopted, it has been broadly used to refer to populations who identify as other than non-Hispanic white: Black/African, Hispanic/Latina/o/x/e, Asian/Pacific Islander, American Indian/Native Alaskan, Indigenous Australian, Middle Eastern, or biracial/multiracial [3]. It is also commonly defined as including individuals with Fitzpatrick skin types IV–VI and those who share similar cutaneous characteristics and disorders, as well as reaction patterns to those conditions [3]. As such, these populations often exhibit variations in epidemiology, clinical presentation, disease burden, and quality of life compared with their non-SOC counterparts, often leading to inaccurate diagnoses, reduced patient satisfaction and compliance, suboptimal outcomes, and increased health-related inequities [1,2,3,4,5,6,7]. With increased attention on healthcare disparities over recent years, there has also been a rise in implementation of strategies that support diversity, equity, and inclusion (DEI) [8]. Nonetheless, these efforts have yet to be effectively integrated into dermatology medical education, research, clinical trials, and ultimately, patient care [7, 8]
To gain awareness of emerging trends and implement best practices in the medical field, resources such as peer-reviewed publications and continued medical education courses serve as an ever-growing repository of knowledge for dermatologists [1, 5]. Importantly, these materials aim to inspire organization-led initiatives by providing insights into existing care gaps, methods to address them, and a baseline from which progress can be effectively monitored. As the topics of DEI and SOC gain traction within the dermatology community, it is imperative to synthesize the current literature to identify prevailing care gaps and evaluate past, present, and future initiatives that aim to promote healthcare equity across the United States (USA). In this study, we sought to assess the dermatological unmet needs of patients with SOC, their caregivers, and healthcare professionals (HCPs), and to understand the current landscape of efforts to improve dermatological care.
Methods
A literature review was conducted using the PubMed database to identify unmet dermatological needs of populations with SOC across the USA from January 2020 to October 2023. Articles were filtered on the basis of specific keywords related to subpopulations, indications, and stakeholders. The full list of search term combinations and the corresponding number of publications can be found in Supplementary Table S1. The literature review yielded 12,159 publications, which were further streamlined to remove duplicates as well as articles that reported findings outside of the USA. Titles and abstracts of articles that did not focus on the dermatological care for patients with SOC were also removed. This detailed review process identified 119 publications, which were then analyzed to extract relevant dermatological care gaps and grouped into four distinct categories of root causes. Importantly, the discrepancy in number of publications retrieved from PubMed may vary depending on the timing of the search, even when consistent search criteria are applied. This variation can be attributed to ongoing updates to the database, including the addition of newly published articles, indexing delays, or changes in PubMed’s search algorithms and indexing practices over time. Additionally, articles may be retracted, corrected, or removed, and shifts in the inclusion of journals may further contribute to changes in search results.
Next, an initiative scan was conducted to evaluate efforts focused on addressing gaps in the dermatological care of patients with SOC within the specified time period. Resulting initiatives (e.g., awards, congresses, curricula, campaigns, and events) were then classified by type of organization (e.g., medical society, state-level societies and SOC centers, pharmaceutical industry, and patient organizations) and assessed for their relevance to each literature-identified care gap. An overview of the search criteria used for the literature review and initiative scan is displayed in Supplementary Fig. S1.
Ethical Approval
This article is based on previously published studies and does not include any new research involving human participants or animals conducted by the authors.
Results
Root Causes of Identified Care Gaps
The comprehensive literature review yielded 18 dermatological care gaps, which were further grouped by the authors into four distinct root causes: cultural diversity, socioeconomic disadvantage, racial and ethnic biases, and underrepresentation in medical research and training (Figure 1: Root causes extracted from identified care gaps for individuals with SOC in the USA. HCP healthcare professional, SOC skin of color)

Next, publications were analyzed to extract the field (i.e., education, research, or healthcare/access) responsible for addressing the identified care gaps and the associated stakeholders (i.e., dermatologists, patients, residents, researchers, and/or caregivers) (Figure 2: Overview of 18 distinct care gaps identified for patients with SOC across dermatology education, research, and clinical care. AI artificial intelligence, HCP healthcare professional, SOC skin of color). These details were either derived explicitly from the publications or implied on the basis of the proposed solutions and future directions.
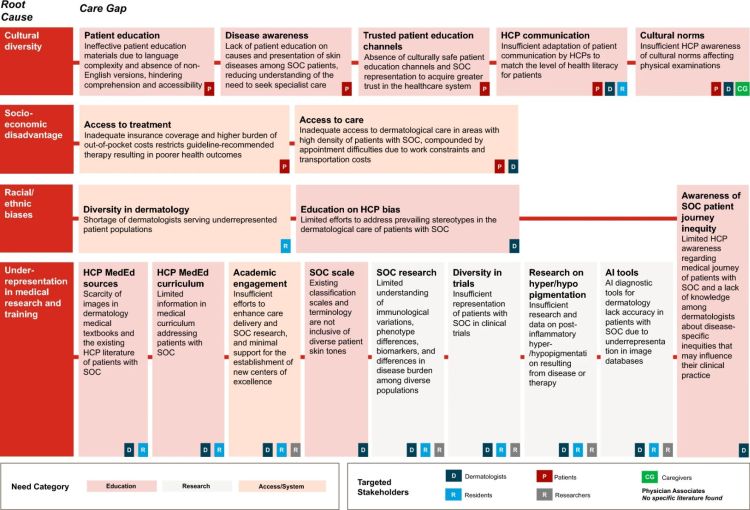
Cultural diversity contributed to gaps in dermatology education, including lack of materials for non-English speakers, absence of culturally sensitive channels for disease awareness, and limited HCP adaptation to health literacy levels of patients [9,10,11,12,13,14,15,16,17]. Additionally, certain populations with SOC may have existing mistrust in the healthcare system, further contributing to their reluctance to seek treatment and understand their condition and exacerbating their fear of side effects. Even if individuals with SOC were trusting of the healthcare system, communication about dermatologic diseases could be hindered by HCPs’ limited familiarity with the disproportionate effects of dermatologic diseases on these patient populations.
Socioeconomic disadvantages exacerbate dermatological healthcare gaps, such as insufficient insurance coverage and restricted access to care in socioeconomically disadvantaged areas, compounded with work constraints and transportation costs [7, 18,19,20,21,22,23,24,25,26]. Populations with SOC may reside in low-income communities with limited healthcare facilities and specialists, resulting in reduced access to advanced technologies. Even when such services are available, costs may be prohibitive, requiring patients to pay high out-of-pocket fees for consultations and treatments and take time off from their jobs to attend medical appointments.
Racial and ethnic biases led to gaps in both dermatology education and healthcare, including a lack of awareness about disease-specific inequities and a shortage of SOC-specialized clinicians, respectively [1, 8, 27,28,29]. Patient trust and satisfaction are closely linked to dermatologists’ awareness of racial and ethnic considerations, as well as cultural sensitivity during patient interactions. Indeed, HCP knowledge and experience with managing patients with SOC have been reported as crucial factors for delivery of culturally competent care [1, 5].
Lastly, gaps arising from underrepresentation in medical and research settings included scarcity of images in dermatology textbooks, insufficient diversity education in medical school, and lack of comprehensive SOC scale to classify diverse patient skin tones. Additionally, numerous limitations have been identified in research, such as lack of nuanced understand of disease burden and clinical presentation across diverse populations, poor representation of individuals with SOC in clinical trials, and low accuracy of artificial intelligence (AI)-based diagnostic tools due to the underrepresentation of patients with SOC in image databases [1,2,4,6,7,13,14,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51].
Identified Initiatives
Following the identification of care gaps, an initiative scan was conducted to evaluate the breadth and focus of activities aimed at mitigating the disparities in dermatological care of individuals with SOC. Thorough review of the landscape of dermatology-specific efforts on the basis of results from the literature review revealed hundreds of initiatives spanning national and international organizations, including medical societies, the pharmaceutical industry, patient advocacy organizations, and nonprofit organizations (Figure 3: SOC-related initiatives arising from the literature search and grouped by societies, industry, and patient organizations. AI artificial intelligence, HCP healthcare professional, MedEd medical education, SOC skin of color).
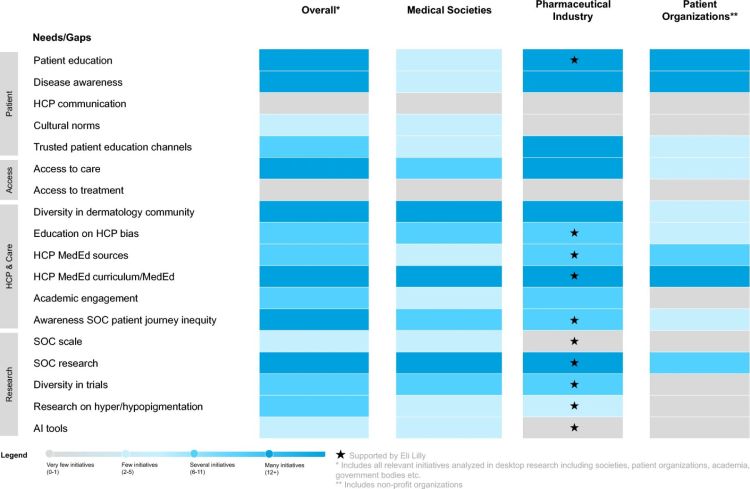
A predominant focus of these initiatives is patient education, with significant efforts dedicated to simplifying materials to enhance comprehension and accessibility for individuals with varying levels of health literacy. In regions with a high density of individuals with SOC, multiple initiatives are underway to improve access to dermatological care by addressing systemic barriers such as work constraints, transportation costs, and limited appointment availability. In response to the shortage of dermatologists serving underrepresented communities, an increasing number of initiatives focus on promoting diversity within the dermatology profession, including scholarships, mentorship programs, and targeted recruitment strategies. Additionally, there is a growing emphasis on raising awareness of disease-specific inequities experienced by patients with SOC, particularly regarding delayed diagnoses and limited availability of culturally competent care. Beyond workforce diversification, there has been a notable push for initiatives that advance research into dermatological conditions affecting populations with SOC, including investigations into immunological variations and phenotypic differences that influence disease presentation, treatment response, and long-term outcomes.
Despite these promising developments, critical areas of improvement remain. For example, many initiatives have yet to adequately address barriers related to effective patient–HCP communication, including the need to develop cultural competence and an improved understanding of the sociocultural factors that influence patient experiences and treatment adherence. Few initiatives have tackled the development of standardized classification systems and terminology that accurately reflect diverse skin tones, and even fewer have explored the integration of AI tools designed to enhance diagnostic accuracy for patients with SOC.
Discussion
In this study, the identified care gaps and their root causes provide a representative snapshot of the dermatological health disparities affecting populations with SOC in the USA. Additionally, mapping of the current landscape of initiatives designed to address these inequities offers valuable insight into existing efforts and helps guide future strategies. The latter will require a collaborative, multi-stakeholder effort, involving HCPs, policymakers, hospital systems, healthcare administrators, medical schools, pharmaceutical companies, and patient advocacy groups.
Within academic settings, it will be crucial to continue to integrate culturally competent dermatology education into medical curricula. This training will help medical students and graduate trainees recognize key cognitive factors, including mistrust, unconscious bias, and stereotyping, while promoting awareness of the multifactorial causes of health disparities and offering tools for effective communication across cultures, languages, and literacy levels. To mitigate potential barriers to care, the dermatology community should further promote the role of patient navigators, who provide essential support with insurance coverage, prescription refills, referrals, and appointment scheduling. Similarly, the use of professional interpreters and linguistic services should be strongly encouraged for all non-English-speaking patients. Policymakers and healthcare administrators should collaborate to allocate funding and resources toward community outreach programs that improve dermatological healthcare access in underserved populations. Medical schools and hospital systems should also partner with patient advocacy groups to co-develop initiatives that address specific concerns from patients with SOC and promote long-term health equity.
Educational content should emphasize the nuances of assessing differences in disease presentation across various skin tones [66]. For example, it is important to convey the original intent of the Fitzpatrick skin type (FST) classification system, which was designed to assess the skin’s propensity to burn during phototherapy, rather than inaccurately using it as a proxy for skin tone. Indeed, the need for more culturally appropriate and clinically relevant tools for measuring skin color warrants further exploration [66]. Despite its limitations as a measure of skin pigmentation, FST is frequently utilized by AI algorithms, often leading to biases and inaccuracies that fail to account for diverse skin tones [67, 68]. Coupled with limited representation of dark skin tones in clinical image datasets, these challenges highlight the need for more research to enhance diagnostic accuracy and clinical decision-making in dermatology for populations with SOC.
From an organizational perspective, pharmaceutical companies also have a responsibility to design clinical trial protocols that recruit and retain participants with diverse skin types [66]. Furthermore, they must ensure equitable access to medications and work with government agencies to implement policies that reduce financial barriers and improve healthcare delivery, especially to underserved communities. Moreover, medical associations should continue to develop opportunities for students from underrepresented groups, reflecting the diverse population of the USA [69].
Importantly, this review is the first of its kind, shedding light on the unmet dermatological needs, existing solutions, and emerging opportunities to improve dermatological care for populations with SOC. While this work provides an abundance of valuable information, certain limitations must be acknowledged. The exclusive use of PubMed as a search engine may have introduced selection bias, potentially leading to an incomplete representation of the available literature. Additionally, while effort was made to ensure comprehensive coverage, the selected search terms may not have fully captured all relevant publications. Moreover, this study focused primarily on cataloguing the quantity of initiatives, without evaluating their real-world impact or long-term efficacy. Future research should assess the effectiveness of these initiatives in reducing disparities, improving patient outcomes, and fostering more equitable access to dermatological care over a longer timeframe to offer a more comprehensive analysis. As part of the initiative scan, websites of relevant dermatological societies and patient organizations were reviewed; however, given the dynamic nature of this landscape, not all initiatives may have been publicly available or uniformly documented, with some organizations maintaining more regularly updated websites than others. Despite these limitations, the broad scope of publications and initiatives analyzed in this review provides a representative snapshot of the current landscape of SOC care in the USA. By establishing a strong foundation, this work enables continued monitoring of progress and informs future efforts to address gaps in the dermatological care of historically underserved populations.
Conclusions
In this review, we shed light on the numerous dermatological care gaps that exist for patients with SOC in the USA and identified initiatives put in place to address them. Despite hundreds of initiatives aimed to address these care gaps, several still require significant attention, particularly in the areas of HCP communication, cultural norms, skin color/type classification scales, and accuracy of AI diagnostic tools for patients with SOC. Although numerous initiatives have sought to address disparities in dermatological care and health outcomes of populations with SOC in the USA, more targeted, evidence-based engagement is required. Specifically, there is a need to understand the impact of initiatives via measurable changes in clinical outcomes, coordinate activities as not to duplicate efforts, and address the root causes underlying the problems. Ultimately, this study aims to inspire practical and scalable initiatives by proposing an iterative framework for evaluation of existing care gaps and periodic assessment of the outcomes attained from these actions to improve access and quality of dermatological care for populations with SOC in the USA.
Data Availability
No datasets were generated or analyzed for this study; therefore, data sharing is not applicable.
References
See the original publication or download the PDF for all references >







